-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 6 Issue 6
Outcome of a rabbit model for late irradiation effects in mandibular oral mucosa and bone: a pilot study
R. Helmers*, D.M.J. Milstein, N.F. Straat, H.M. Rodermond, N.A.P. Franken, C.D. Savci-Heijink, H.H. de Boer, J. de Lange
Helmers et al. J Clin Transl Res 2020; 6(6):5
Published online: December 11, 2020
Abstract
Background/Aim/Objective: Late side effects of radiotherapy (RT) in the treatment for head and neck (HN) malignancies involve an inadequate healing response of the distressed tissue due to RT induced hypovascularity. The aim of this study was to develop a pilot model in which vascular alterations associated with the onset of late irradiation (IR) injury could be measured in rabbit oral mucosa and mandibular bone.
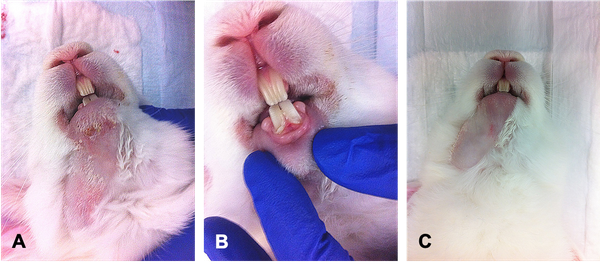
Materials and methods: Eight male New Zealand White rabbits were divided over 4 treatment groups. Group I-III received 4 fractions of RT (5.6 Gy, 6.5 Gy and 8 Gy respectively) and group IV received 1 fraction of 30 Gy. Oral microcirculatory measurements were performed at baseline (before RT) and once a week during 11 consecutive weeks after RT assessing perfusion parameters, i.e. total vessel density (TVD), perfused vessel density (PVD), proportion of perfused vessels (PPV) and microvascular flow index (MFI). Post-mortem histopathology specimens were analyzed.
Results: Five weeks after RT, TVD and PVD in all groups showed a decrease of >10% compared to baseline, a significant difference was observed for groups I, II and IV (p<0.05). At T11 no lasting effect of decreased vessel density was observed. PPV and MFI remained unaltered at all time points. Group IV showed a marked difference in scattered telangiectasia-like microangiopathies, histological necrosis and loss of vasculature.
Conclusion: No significant lasting effect in mucosal microcirculation density due to IR damage was detected. Observed changes in microcirculation vasculature and histology may align preliminary tissue transition towards clinical pathology in a very early state associated with late IR injury in the oral compartment.
Relevance for patients: Enhancing knowledge on the onset of late vascular IR injury in the HN region could help the development, monitoring and timing of therapies that act on prevention, discontinuation or repair of radiation pathology.
DOI: http://dx.doi.org/10.18053/jctres.06.202006.005
Author Affiliation
1. Department of Oral and Maxillofacial Surgery, Amsterdam University Medical Centre (UMC), Location: AMC, University of Amsterdam, Meibergdreef 9, 1105 AZ, Amsterdam, The Netherlands
2. Academic Centre for Dentistry Amsterdam, University of Amsterdam and VU University, Gustav Mahlerlaan 3004, 1081 LA, Amsterdam, The Netherlands
3. Laboratory of Experimental Oncology and Radiobiology, Amsterdam UMC, Location: AMC, University of Amsterdam, Meibergdreef 9, 1105 AZ, Amsterdam, The Netherlands
4. Department of Radiation Oncology, Amsterdam UMC, Location: AMC, University of Amsterdam, Meibergdreef 9, 1105AZ Amsterdam, The Netherlands
5. Department of Pathology, Amsterdam UMC, Location: AMC, University of Amsterdam, Meibergdreef 9, 1105 AZ, Amsterdam, The Netherlands
*Corresponding author
Renée Helmers
Department of Oral and Maxillofacial Surgery Amsterdam University Medical Centre, Location AMC, University of Amsterdam, Meibergdreef 9, 1105 AZ, Amsterdam, The Netherlands
Tel: +31-20-566-5265
Fax: +31-20-566-9032
Email: R.Helmers@amsterdamumc.nl
Handling editor:
Ammar Musawi
A T Still University, Jefferson, United States

