-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 7 Issue 5
Tagging incidental finding of fatty liver on ultrasound: A novel intervention to improve early detection of liver fibrosis
Navroop Nagra*, Rubal Penna, Danielle La Selva, David Coy, Asma Siddique, Blaire Burman
Nagra et al. J Clin Transl Res 2021; 7(5):9
Published online: September 29, 2021
Abstract
Background: It is not uncommon to see that a large proportion of patients with cirrhosis due to Nonalcoholic steatohepatitis (NASH) never had any prior evaluation or diagnosis of liver disease, and most of the times their first clinical presentation is decompensated cirrhosis. Acknowledging incidental finding of fatty liver on abdominal imaging and identifying patients at risk of having advanced liver fibrosis may help in preventing its progression to cirrhosis.
Aim: We aimed to increase acknowledgement and improve evaluation of steatosis via radiology recommendation to consider hepatology referral, and to identify the predictors of hepatology referral and significant fibrosis.
Methods: We performed a retrospective study of 812 patients with hepatic steatosis tagged on ultrasound (US), over 18 months, at a single center. Patients with secondary causes of fatty liver were excluded. We evaluated the yield of this intervention and factors correlated with hepatology referral and presence of significant fibrosis.
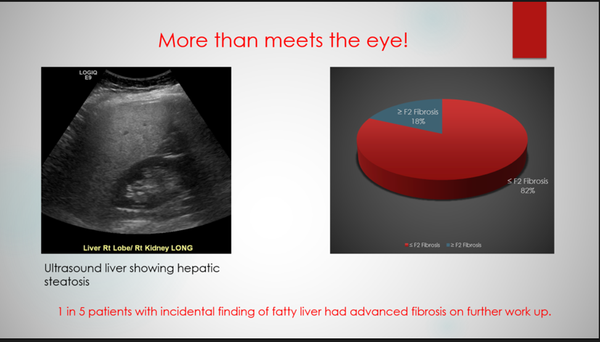
Results: Diagnosis of fatty liver was acknowledged for 69% of patients with tagged US, although only 29% were ultimately seen by hepatology. Patients who had US ordered by a primary care provider (PCP) were more likely to have hepatology evaluation (64.8% vs 56.9%, P = 0.0183). Sixty-six percent of patients seen by hepatology had elevated alanine transaminase (ALT) compared to 52% not seen by hepatology (P < 0.0005). Among patients further evaluated, 53% underwent staging, and 18% had ≥ stage 2 (F2) fibrosis. Type II diabetes (DMII) correlated with significant to advanced fibrosis (43.5% vs 21.4%, P = 0.0357), while ALT and Body Mass Index (BMI) did not.
Conclusions: Tagging US reports led to clinical acknowledgement of fatty liver in 7 of 10 patients, although fewer than 1 in 3 had further hepatology evaluation. Of those who underwent staging for incidentally noted steatosis, 18% had significant fibrosis, suggesting that we are failing to evaluate patients with potentially advanced liver disease.
Relevance for patients: Identifying incidental finding of fatty liver on US provides a unique opportunity in diagnosing liver fibrosis at an early stage and can help prevent its progression to cirrhosis. Primary care providers should consider using noninvasive scoring systems on a regular basis to assess the risk of fibrosis in patients with fatty liver, and timely referral to hepatology should be provided in patients at high risk of having advanced fibrosis.
DOI: http://dx.doi.org/10.18053/jctres.07.202105.009
Author affiliation
1. Digestive Disease Institute, Virginia Mason Medical Center, Seattle, WA 98101, United States
2. Department of Radiology, Virginia Mason Medical Center, Seattle, WA 98101, United States
*Corresponding author
Navroop Nagra
Digestive Disease Institute, Virginia Mason Medical Center, 1100 Ninth Ave, Seattle, WA 98101, United States
Tel: 530-701-5116
Email: nagra.navi24@gmail.com
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

