-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 8 Issue 6
Tumor grade and symptoms at presentation are survival risk factors in Chinese patients with primary retroperitoneal sarcoma
Aobo Zhuang, Yuan Fang, Michal Heger, Lijie Ma, Jing Xu, Jiongyuan Wang, Weiqi Lu, Hanxing Tong, Yuhong Zhou*, Yong Zhang*
Zhuang et al. J Clin Transl 2022; 8(6):16
Published online: November 24, 2022
Abstract
Background and aim: No cohort studies have been performed on Chinese primary retroperitoneal sarcoma (RPS) patients. Data derived from Western cohort studies may not be directly superimposable on Asian counterparts. Furthermore, the risk factors for survival of RPS are currently unknown for Chinese patients. The objectives were therefore to (1) gain insight into RPS incidence and patient demographics and clinical details; (2) determine the risk factors for overall survival (OS) and disease-free survival (DFS); and (3) critically appraise the Asian cohort data in relation to information obtained in Wester cohort studies.
Methods: In this retrospective cohort study, the health records of patients that had been diagnosed with primary localized RPS with curative intent between 2009 and 2020 were analyzed. Cox proportional hazards analysis was conducted to evaluate the risk factors for OS and DFS.
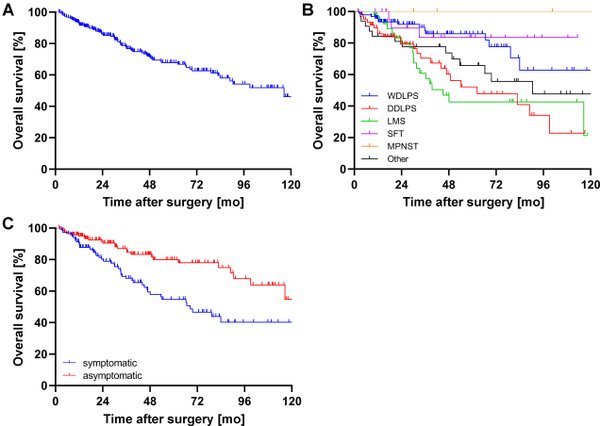
Results: A total of 261 patients met the inclusion criteria. Ninety-six (36.8%) patients had been diagnosed with well-differentiated liposarcoma, 63 patients (24.1%) with dedifferentiated liposarcoma, 41 patients (15.7%) with leiomyosarcoma (LMS), 22 patients (8.4%) with solitary fibroma, 7 patients (2.7%) with malignant peripheral nerve sheath tumor (MPNST), and 32 patients (12.3%) with another type of RPS. The study further revealed that (1) the 5-y OS and DFS in RPS patients was 67.8% and 51.3%, respectively, with the highest OS and DFS observed in MPNST (100% and 100%, respectively) and the lowest 5-y OS and DFS attributed to LMS (42.6% and 28.9%, respectively); (2) symptoms at presentation, FNCLCC grade, and number of combined resections are independent risk factors in OS; (3) symptoms at presentation, FNCLCC grade, chemotherapy, and hospital length of stay are independent risk factors for DFS; and (4) patients at high risk (symptoms at presentation and high-grade tumors) have less than half the chance of survival at 5 y post-diagnosis than patients with a low-risk profile.
Conclusions: Symptoms at presentation constitute a risk factor for OS and DFS. When combined with tumor grade - another risk factor for both OS and DFS - patients can be classified into a high-risk and low-risk category to gauge a patient’s prognosis and, accordingly, frame an optimal clinical trajectory. Moreover, the clinicopathology and overall prognosis of RPS in Asian and Western populations are comparable and hence superimposable.
Relevance for patients: The present study identifies the risk factors of survival in RPS and suggests symptoms at presentation should be considered in the preoperative consultation and added in prognostic grouping.
DOI: http://dx.doi.org/10.18053/jctres.08.202206.016
Author affiliation
1. Department of General Surgery, Zhongshan Hospital, Fudan University, Shanghai, China
2. Xiamen University Research Center, Retroperitoneal Tumor Committee of Oncology Society of Chinese Medical Association, Xiamen University, Xiamen, Fujian, China
3. Department of General Surgery, South Hospital of the Zhongshan Hospital/Shanghai Public Health Clinical Center, Fudan University, Shanghai, China
4. Department of Gastrointestinal Surgery, Shanghai General Hospital Affiliated to Shanghai Jiaotong University, Shanghai, China
5. Jiaxing Key Laboratory for Photonanomedicine and Experimental Therapeutics, Department of Pharmaceutics, College of Medicine, Jiaxing University, Jiaxing, Zhejiang, China
6. Laboratory Experimental Oncology, Department of Pathology, Erasmus MC, Rotterdam, the Netherlands
7. Department of Medical Oncology, Zhongshan Hospital, Fudan University, Shanghai, China
*Corresponding authors
Yong Zhang
Department of General Surgery, Zhongshan Hospital, Fudan University, 180 Fenglin Road, Shanghai, China
Tel: +86 21 64041990
Email: 13681971072@163.com
Yuhong Zhou
Department of Medical Oncology, Zhongshan Hospital, Fudan University, 180 Fenglin Road, Shanghai, China
Tel: +86 21 64041990
Email: zhou.yuhong@zs-hospital.sh.cn
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

