-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 9 Issue 4
PD-L1 expression and prognosis in definitive radiotherapy patients with neuroendocrine cervical carcinoma
Huiling Li*, Xiuhua Li, Meichun Yang, Huiyan Su, Jianqiu Zhang, Chunmiao Hu, Yingming Sun, Dan Hu, Li Chen
Li et al. J Clin Transl Res 2023; 9(4):23-00067
Published online: July 28, 2023
Abstract
Background: Neuroendocrine carcinoma of the cervix (NECC) is more prone to lymphatic infiltration, lymph node involvement, local recurrence, and distant metastasis. Using CCRT with or without adjuvant chemotherapy as the standard treatment for locally advanced NECCs and CCRT for patients with early lesions confined to the cervix. However, the prognosis of NECC patients treated with definitive radiotherapy (RT) is unknown. Immune checkpoint inhibitors are a promising therapeutic strategy for locally advanced cervical cancer. Some reports suggest that the expression of PD-L1 in solid tumors correlates with prognosis.
Aim: This study investigates prognostic factors for survival in patients with neuroendocrine cervical carcinoma (NECC) treated with definitive radiotherapy (RT) and the relationship between PD-L1 expression and prognosis in these patients.
Methods: This retrospective study included 66 patients with histologically confirmed NECC who received RT with or without chemotherapy. From January 2015 to December 2020, patients received routine extended-field irradiation (EFI), and PD-L1 expression was assessed by immunohistochemistry. The most commonly used chemotherapy agents were etoposide-platinum and paclitaxel-platinum.
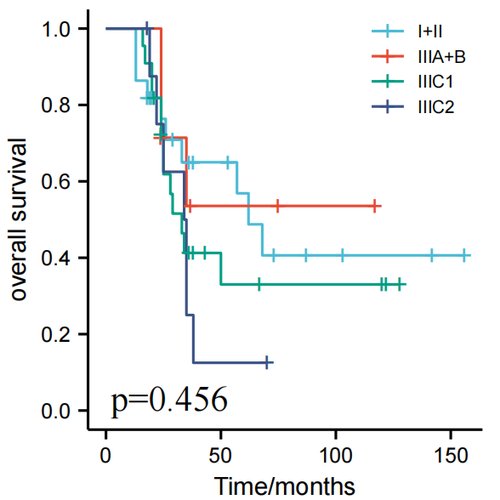
Results: PD-L1 expression was positive in 17 of 45 (37.8%) patients. There were 52 cases of pure NECC and 14 cases of mixed carcinoma. Sixty stage IB-III patients received definitive RT. The 3- and 5-year progression-free survival (PFS) was 39.8% and 34.1%, and 3- and 5-year overall survival (OS) was 48.0% and 40.2%, respectively. There was no significant difference in 3 and 5-year PFS and 3 and 5-year OS between patients with pure and mixed carcinoma. Positive PD-L1 expression was associated with higher 3-year PFS in patients with mixed histology. Univariate analysis showed that LNM and FIGO stages predicted 3-and 5-year PFS in patients who received definitive RT. The median OS in patients receiving less than four cycles and at least four cycles of chemotherapy (CT) was 26.0 and 44.0 months, respectively (P=0.038); moreover, 3- and 5-year PFS was 34.1% and 25.7% in the former and 46.4% and 40.4% in the latter. There were no significant differences in OS and PFS between pelvic irradiation and prophylactic EFI in patients treated with definitive RT. There were no significant differences in para-aortic failure rate after concurrent chemoradiotherapy between patients who underwent pelvic irradiation or prophylactic EFI (p=0.147).
Conclusion: In patients with mixed NECC, positive PD-L1 expression is correlated with higher 3-year PFS. Chemoradiotherapy was effective for NECCs. The LNM and stage predicted PFS. Four or more cycles of chemotherapy improve prognosis. Prophylactic EFI did not significantly improve PFS and OS.
Relevance for patients: This study is relevant to patients as it confirms that chemoradiotherapy is effective for both early and locally advanced NECC, and that four or more cycles of chemotherapy improved prognosis. The regimen should be carefully evaluated to ensure that patients receive the most effective radiation therapy for the prophylactic of para-aortic lymph node metastasis. Potential risk factors for recurrence of radical radiotherapy should be fully understood to minimize these risks. This study observed that PD-L1 expression positive in patients with mixed NECC types is correlated with higher 3-year PFS.
DOI: http://dx.doi.org/10.18053/jctres.09.202304.23-00067
Author affiliation
1. Department of Gynecology, Clinical Oncology School of Fujian Medical University, Fujian Cancer Hospital, Fuzhou, Fujian, China
2. Department of Radiology, Clinical Oncology School of Fujian Medical University, Fujian Cancer Hospital, Fuzhou, Fujian, China
3. Department of Radiotherapy, Affiliated Sanming First Hospital, Fujian Medical University, Sanming, Fujian, China
4. Department of Pathology, Clinical Oncology School of Fujian Medical University, Fujian Cancer Hospital, Fuzhou, Fujian, China
5. School of Arts and Sciences, Fujian Medical University, Fuzhou, Fujian, China
*Corresponding author
Huiling Li
Department of Gynecology, Clinical Oncology School of Fujian Medical University, Fujian Cancer Hospital, Fuzhou, Fujian, China.
E-mail: huilin888999@126.com
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Chemistry, Utrecht University, Utrecht, the Netherlands
Department of Pathology, Erasmus Medical Center, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

