-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 7 Issue 1
A pilot, randomized controlled trial of telementorship: A useful tool during social distancing
Nicolas D. Prionas, Tiffany H. Kung, Ann Dohn, Nancy Piro, Rie von Eyben, Laurence Katznelson, Thomas J. Caruso*
Prionas et al. J Clin Transl Res 2021; 7(1):2
Published online: January 20, 2021
Abstract
Background: During social distancing, resident mentorship may be an unmet need. Tele-mentorship, mentorship via video-conferencing software, presents a unique approach to overcome these challenges.
Aims: This study evaluated whether tele-mentorship via video-conference increased access to mentorship encounters and decreased perceived barriers to access, factors that determine likelihood to maintain mentor relationships, and quality of mentorship.
Methods: A year-long randomized, prospective cohort study was conducted in 2016 to 2017 with pairs of resident mentors from seven different training programs and medical student mentees, randomized to tele-mentorship or in-person mentorship. The number of quarterly encounters was monitored and demographic predictors of meeting were determined. Likert scale survey responses were analyzed with linear regression.
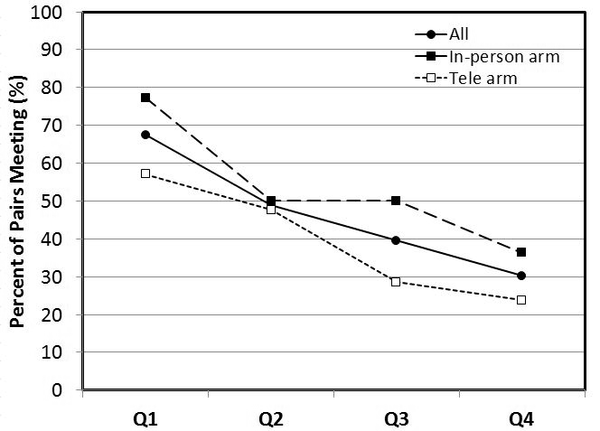
Results: Forty-three of forty-six (93.5%) volunteer mentor-mentee pairs participated. Tele-mentorship did not alter likelihood of meeting or attitudes toward mentorship barriers (time, distance). Mentee satisfaction increased from 42.5% to 65.4% (p<0.05) throughout the year. Operating room-based practice (p<0.05) and higher postgraduate level (p=0.02) decreased the likelihood of meeting.
Conclusions: Tele-mentorship provided an equal number of encounters compared to the pairs who were asked to meet in-person. Tele-mentorship may serve as an adjunct modality for flexible communication.
Relevance for Patients: Medical mentorship is a key component to medical education. Effective mentorship increases academic research productivity, job satisfaction, and advancement of clinical skills, which translate to improved patient care.
DOI: http://dx.doi.org/10.18053/jctres.07.202101.002
Author affiliation
1. Department of Radiation Oncology, University of California San Francisco Medical Center 505 Parnassus Ave. San Francisco, CA 94143
2. Department of Anesthesiology, Perioperative, and Pain Medicine, Massachusetts General Hospital, 55 Fruit Street, Boston, MA, 02114
3. Department of Graduate Medical Education, Stanford University Medical Center
300 Pasteur Drive - Room HC435, Stanford, CA 94305-5207
4. Department of Radiation Oncology, Stanford Cancer Center, MC 5847, 875 Blake Wilbur Drive Stanford, CA 94305-5847
5. Department of Medicine, Stanford University Medical Center, 300 Pasteur Drive - Room S102, Stanford, CA 94305-5110
6. Department of Neurosurgery, Stanford Neuroscience Health Center, 213 Quarry Road, Palo Alto CA 94304-5979
7. Department of Anesthesiology, Perioperative, and Pain Medicine, Stanford University Medical Center, 300 Pasteur Drive, H3584 Stanford, CA 94305-5640
*Corresponding Author
Thomas Caruso
Department of Anesthesiology, Perioperative, and Pain Medicine. Stanford University Medical Center, 300 Pasteur Drive, H3584 Stanford, CA 94305-5640
Email: tjcaruso@stanford.edu
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

