-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 1 Issue 2
Laser-assisted vessel welding: state of the art and future outlook
Dara R. Pabittei, Wadim de Boon, Michal Heger, Rowan F. van Golen, Ron Balm, Dink A. Legemate, Bas A. de Mol
Pabittei et al., J Clin Transl Res, 2015; 1(2): 61-77
Published online: 30 September, 2015
Abstract
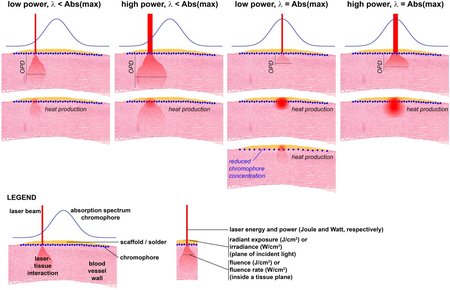
Laser-assisted vascular welding (LAVW) is an experimental technique being developed as an al-ternative to suture anastomosis. In comparison to mechanical anastomosis, LAVW is less traumatic, non-immunogenic, provides immediate watertight sealant, and possibly a faster and easier procedure for minimally invasive surgery. This review focuses on technical advances to improve welding strength and to reduce thermal damage in LAVW. In terms of welding strength, LAVW has evolved from the photothermal-induced microvascular anastomosis, requiring stay sutures to support welding strength, to sutureless anastomoses of medium-sized vessels, withstanding physiological and supraphysiological pressure. Further improvements in anastomotic strength could be achieved by the addition of chromophore-containing albumin solder and the employment of (biocompatible) polymeric scaffolds. The anastomotic strength and the stability of welds achieved with such a modality, referred to as scaffold- and solder-enhanced LAVW (ssLAVW), are dependent on the intermolecular bonding of solder molecules (cohesive bonding) and the bonding between solder and tissue collagen (adhesive bonding). Presently, the challenges of ssLAVW include (1) obtaining an optimal balance between cohesive and adhesive bonding and (2) minimizing thermal damage. The modulation of thermodynamics during welding, the application of semi-solid solder, and the use of a scaffold that supports both cohesive and adhesive strength are essential to improve welding strength and to limit thermal damage.
DOI: http://dx.doi.org/10.18053/jctres.201502.006
Author affiliation
1 Department of Cardiothoracic Surgery, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands
2 Department of Surgery, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands
3 Department of Physiology, Hasannuddin University Faculty of Medicine, Makassar,South Sulawesi, Indonesia
4 Department of Experimental Surgery, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands
5 Department of Biomedical Engineering, Material Technology, Technical University Eindhoven, Eindhoven, The Netherlands
*Corresponding author:
Bas A. de Mol
Biomedical Engineering, Materials Technology, PO Box 513, WH 4.110, 5600 MB Eindhoven, The Netherlands
Tel: +31 40 247 4063
E-mail: b.a.j.m.d.mol@tue.nl
Handling editor:
Guillermo AguilarDepartment of Mechanical Engineering, University of California at Riverside, Riverside, CA, United States

