-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 1 Issue 2
Platelet aggregation but not activation and degranulation during the acute post-ischemic reperfusion phase in livers with no underlying disease
Rowan F. van Golen, Katarzyna M. Stevens, Pina Colarusso, Hartmut Jaeschke, Michal Heger
van Golen et al., J Clin Transl Res, 2015; 1(2): 107-115
Published online: 13 September, 2015
Abstract
Background: Platelets and P-selectin (CD62P) play an unequivocal role in the pathology of hepatic ischemia/reperfusion (I/R) injury. Inhibition or knock-out of P-selectin or immunodepletion of platelets results in amelioration of post-ischemic inflammation, reduced hepatocellular damage, and improved survival. However, P-selectin expression on platelets and endothelial cells, which concurs with platelet activation, has never been clearly demonstrated in I/R-subjected livers.
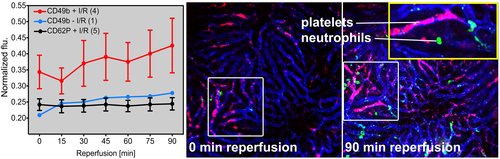
Aims: To determine whether platelets become activated and degranulate in the acute phase of liver I/R and whether the platelets interact with neutrophils.
Methods: Hepatic I/R was induced in male C57BL/6J mice (N = 12) using 37.5-min ischemia time. Platelets, endothelial cells, and neutrophils were fluorescently labeled by systemic administration of non-blocking antibodies. Cell kinetics were monitored by intravital spinning disk confocal mi-croscopy during 90 min of reperfusion. Image analysis and quantification was performed with dedicated software.
Results: Platelets adhered to sinusoids more extensively in post-ischemic livers compared to livers not subjected to I/R and formed aggregates, which occurred directly after ischemia. Platelets and endothelial cells did not express P-selectin in post-ischemic livers. There was no interaction between platelets and neutrophils.
Conclusions: Platelets aggregate but do not become activated and do not degranulate in post-ischemic livers. There is no platelet-neutrophil interplay during the early reperfusion phase in a moderate model of hepatic I/R injury. The mechanisms underlying the biological effects of platelets and P-selectin in this setting warrant further investigation.
Relevance for patients: I/R in surgical liver patients may compromise outcome due to post-ischemic oxidative stress and sterile inflammation. Both processes are mediated in part by platelets. Under-standing platelet function during I/R is key to developing effective interventions for I/R injury and improving clinical outcomes.
DOI: http://dx.doi.org/10.18053/jctres.201502.001
Author affiliation
1 Department of Experimental Surgery, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands
2 Live Cell Imaging Facility, Snyder Institute for Chronic Diseases, University of Calgary, Calgary, Alberta, Canada
3 Department of Pharmacology, Toxicology and Therapeutics, University of Kansas Medical Center, Kansas City, USA
*Corresponding author:
Michal Heger
Department of Experimental Surgery, Academic Medical Center Meibergdreef 9, 1105 AZ Amsterdam, The Netherlands
Tel: +31 20 5665573
Email: m.heger@amc.uva.nl
Handling editor:
Yao Liu
Department of Membrane Biochemistry and Biophysics, Utrecht University, The Netherlands

